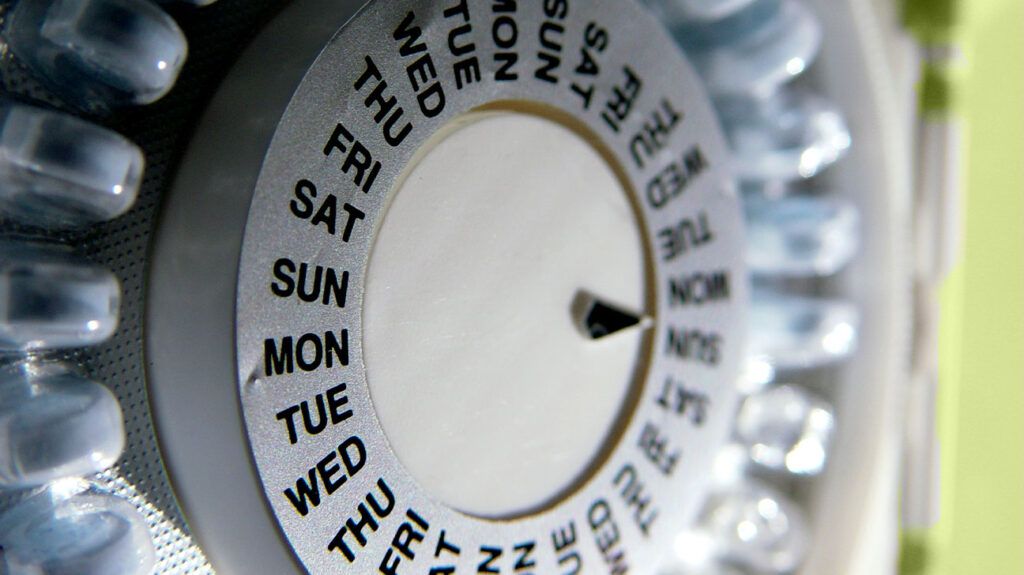
- The combined hormonal contraceptive pill is the second most popular form of contraception in the United States, besides condoms.
- Ethinyl estradiol has been used in the contraceptive pill since it was first created 60 years ago.
- Researchers have discovered that rats given this hormone exhibited more behaviors associated with anxiety, compared to a more natural estrogen used in a more modern form of the contraceptive pill.
Rats given synthetic estrogens used in birth control pills exhibited greater signs of anxiety than those given natural estrogens, researchers have found.
The study showed synthetic estrogens were associated with lower steroid hormone levels when compared to natural ones. The findings, which are not yet published in a peer-reviewed scientific journal, were recently presented at ENDO 2024, the Endocrine Society’s annual meeting in Boston, MA.
The natural estrogen used in this study was similar to the one used in NOMAC-E2, a combined oral contraceptive formulation known as Zoely, which is produced by the pharmaceutical company Merck. The synthetic estrogen used in most combined hormonal contraceptive pills on the market is a highly potent synthetic estrogen called ethinyl estradiol.
Researchers had been looking for natural estrogen to use in combined hormonal contraceptive pills since its inception 60 years ago, but these had not been potent enough for those pills to be an effective form of hormonal contraceptive. This changed in 2011 when Zoely was introduced to the market.
Abigail Hegwood, MS, who carried out the study, told Medical News Today she wanted to investigate the new, natural estrogen on the market as she had become aware there was little epidemiological data on the side effects of specific progestins and estrogens.
“I wanted to know [whether there is] a difference between these two estrogens. They just released this natural estrogen on the market. Does this possibly give us an opportunity to find a difference between formulations in terms of behavioral side effects?”
— Abigail Hegwood, MS, study author
Three groups of 12 female rats were given either ethinyl estradiol a synthetic estrogen with dienogest, a progestin often combined with it in oral combined hormonal contraception, or estradiol valerate a natural estrogen with dienogest, or a control, delivered via a subcutaneous pump for 28 days.
The researchers tested the rats’ spatial awareness and anxiety in a maze test between days 20–28 and collected serum samples on day 28.
The researchers discovered that the rats had similar spatial memory across all three groups.
However, rats that were given the synthetic estrogen had a different response to the spatial memory task in the maze test, which is believed to be associated with anxiety-like behaviors in these animals.
Serum samples also showed that both types of estrogen reduced circulating testosterone.
The authors note levels of estradiol in blood serum were below the detection limit in over half of rats given ethinyl estradiol.
Previous research has shown that higher levels of testosterone and E2 reduce anxiety-related behaviors and improve spatial memory, the authors noted.
They propose that the results they have seen are due to the effect of synthetic estrogens on the brain.
“Ethinyl estradiol and estradiol valerate have different effects on hormone-binding globulin. And hormone-binding globulin can bind and render steroid hormones in the blood unavailable for use by the body. And so we know that ethinyl estradiol increases hormone-binding globulin, which increases the amount of bound steroid hormone in the blood,” Hegwood said.
“So my hypothesis would be that because ethinyl estradiol is having this greater effect on the availability of steroid hormones, it would have a greater effect on the actions that these steroid hormones have on the body, including the brain,” she added.
Hegwood’s supervisor Alesia Prakapenka, PhD, an assistant professor in the Biomedical Sciences program at Midwestern University in Downers Grove, Ill, told MNT:
“Another potential outcome is there’s the feedback loop that’s being halted by the contraceptive treatments between the hypothalamus, the pituitary, and the gonads.”
Naturally-produced circulating estrogen was below the level of detection in many of the rats given ethinyl estradiol.
“What we actually saw is that with the synthetic ethinyl estradiol group, more than half of the samples in that group had 17-beta estradiol levels that were actually below the limit of detection. And so it could be that even if it’s not the hormone itself from the contraceptive, it may be changing something within the feedback loop that then could be having that effect,” Prakapenka explained.
Prakapenka said there hasn’t been much focus on the behavioral effects of hormonal contraception.
“I think bringing this to attention is exciting because now we can start to look at it more and then combine it with additional factors that are across the lifespan could be impacting females, including pregnancy, including menopause,” she said.
Tailored birth control options“There’s a lot of development that’s happening with different options for menopausal hormone therapy. So maybe taking those strategies, applying them to contraceptive use as well, kind of across the board, what a female can go through and how we can inform them of this. These are your options. These are kind of the individual changes that you may experience and how to adjust based on that individual woman, as opposed to women as a whole or females as a whole.”
— Alesia Prakapenka, PhD
While it was possible that combined hormonal contraception could affect the brain and, therefore, behavior, Jonathan Schaffir, MD, vice chair of Education in the Department of Obstetrics and Gynecology at the Ohio State University College of Medicine, who was not involved in the research, said this effect would likely be small.
“There are receptors for estrogens as well as other steroids in the human brain, and we know that providing exogenous hormones can influence mood and behavior to some degree. That said, I think that the influence of oral contraceptives is usually small, and it’s a small percentage of women who have any significant side effects that affect mood,” he told MNT.
“I think that you know, rat behavior is a far cry from human behavior, so looking at more appropriate measures of mood and behavior in humans would be appropriate. But I guess my other takeaway from this study is that it’s always important to examine the components of medications that we use, and to try to include, particularly in the setting of hormonal treatment, the versions of hormones that have the fewest side effects and the best physiologic response.”
— Jonathan Schaffir, MD
“We should also strive to create new medications with better response and fewer side effects,” Schaffir concluded.
