A surgeon may use joint revision surgery to remove and replace failing parts of a total joint replacement. They may recommend it if a person experiences pain, swelling, or stiffness due to a loose or worn artificial joint.
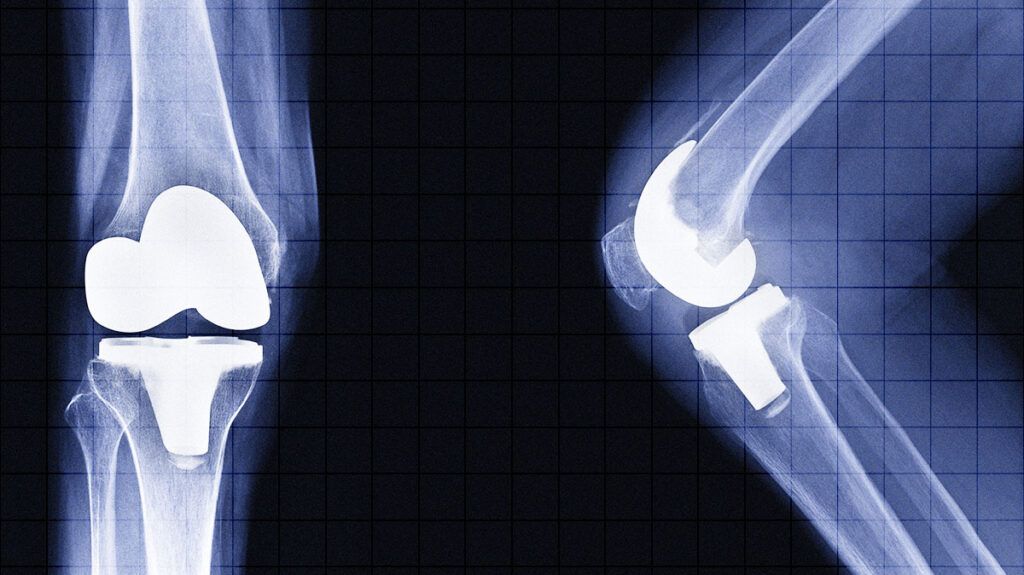
A total joint replacement involves a surgeon replacing cartilage and bone in a joint with a metal and plastic artificial device. Over time, the replacement artificial device may become worn or loose. One or more of the metal and plastic components may need replacing.
Read on to learn more about joint revision surgery. This article looks at what it involves, what it can treat, when a doctor may recommend it, and more.
One of the
To begin joint revision surgery, the surgeon will typically follow the incision line from the original joint replacement surgery to reveal the artificial device. The surgeon can then examine the device and the surrounding bones and tissue to assess the damage and check for signs of infection.
The surgeon can then carefully remove the artificial device, trying not to damage any surrounding bone in the process.
The surgeon may need to remove any cement from the bone that kept the artificial device in place. They may also remove some tissue to send to the laboratory to determine if there is an infection or other cause of device failure.
The surgeon can then prepare the surrounding bones for the replacement device and insert it into the joint.
There may be a loss of bone, which the surgeon may need to replace with extra device components. There may also be damage to the tissue surrounding the joint the surgeon needs to repair.
Doctors
- infection in or around the artificial device
- loosening of the device
- pain
- wear and tear of the artificial device
- instability of the artificial device
- a fracture around the bone
- a breakage of the artificial device
- stiffness of the artificial device
The artificial device may become loose, unstable, stiff, or broken due to factors
- heterotopic ossification, where bone grows as scar tissue around a joint replacement
- incorrect positioning of the implants during prior surgery
- taking part in high impact physical activity or exercise
- obesity
- being of a younger age at the time of the initial joint replacement
- increased life expectancy
According to a
- pain reduction
- reduce stiffness
- increase range of motion
- improve quality of life
However, an older study from 2016 suggests that joint revision surgery may be less effective at reducing pain than the initial joint replacement.
A doctor can provide a person with more information about the possible benefits of joint revision based on their specific circumstances.
In preparation for joint revision surgery, a person may wish to prepare the home for returning from the hospital. This can include:
- precooking meals
- making sure essential items are within easy reach
- purchasing any items, such as mobility devices, that may assist in recovery
A person will require imaging tests before joint revision. These can include X-rays, MRIs, and CT scans. A doctor may also order blood tests to check for signs of infection.
A person may experience mobility restrictions for several weeks following the procedure. Therefore, they may want to arrange for another person to assist them at home with tasks, such as:
- laundry
- bathing
- cooking
- grocery shopping
A person will need to follow wound care instructions to promote healing and avoid infection. A doctor will typically remove the wound staples or stitches several weeks following a joint revision.
A surgeon may recommend physical therapy and rehabilitation exercises for a person to follow.
A doctor may also recommend medications, such as blood-thinning medication and antibiotics, to help prevent blood clots and infections.
Recovery time from joint revision surgery may vary depending on the joint requiring the procedure and the person’s general health.
Recovery may take approximately 3 to 6 months for a person to resume daily activities. It can take up to 12 months to fully recover.
Joint revision is a more complex procedure than the initial total joint replacement. Therefore, the risk of complications may be greater.
Possible complications may include:
- blood clots
- bleeding
- infection within the wound or in the artificial device
- fracture of the bone during the procedure
- nerve or blood vessel damage
- poor healing of the wound site
- heart attack
- stroke
The alternatives to joint revision surgery may be more complex and may not offer the same results.
However, if a person does not want to undergo joint revision surgery, the alternatives may include fusing the joint or amputating the joint and surrounding area.
Fusing the bones in the joint together may limit the joint’s range of motion.
A doctor may only recommend amputating the joint and surrounding areas if a person has a severe infection.
Joint revision surgery can replace all or part of a total joint replacement if the artificial device stops working effectively or a person develops an infection.
A doctor may recommend joint revision if the artificial device has become worn or loose or if a person is experiencing stiffness and pain.
Joint revision surgery is typically more complex than the original joint replacement. It can take up to 12 months for a full recovery.
After a joint revision surgery, a person will typically experience reduced pain, improved mobility, and a better quality of life.
