Metastatic breast cancer (MBC) is breast cancer that has spread to other parts of the body. Treatment depends on various factors, including whether a person is pre- or postmenopausal.
In this article, find answers to eight frequently asked questions about treatments and management strategies for MBC.

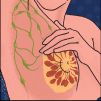
A person’s tumor profile is important in determining their treatment options. The details of the tumor profile indicate which of three types of receptors are present in cancer cells:
- estrogen receptor
- progesterone receptor
- human epidermal growth factor receptor 2, known as the HER2 receptor
If the breast cancer is positive for the estrogen or progesterone receptors, it means that hormones are influencing it. People with MBC at any stage with hormone receptor-positive breast cancer
In premenopausal people with MBC, first-line treatment typically involves tamoxifen (Nolvadex) or an aromatase inhibitor to suppress the ovaries and block hormones.
In postmenopausal people, treatment can include hormonal therapy with an aromatase inhibitor.
As mentioned above, the initial combination of medications for people with cancer that is positive for the estrogen or progesterone receptors depends on the occurrence of menopause.
Chemotherapy
The specific regimen depends on multiple factors, including the use of any previous regimens.
Doctors also consider the medical condition of the person and the presence of any other medical concerns, such as heart disease, before recommending treatment options.
Advances in the treatment of MBC continue to evolve. It is important that people with MBC ask their medical teams whether there are new strategies specific to their tumor type, taking their medical history into consideration.
The tumor profile determines the targeted therapies for which a person with MBC may be a suitable candidate. In those with HER2-positive breast cancer, doctors prescribe medications such as trastuzumab (Herceptin) to counteract the HER2 receptor.
Pertuzumab (Perjeta) is another MBC agent that focuses on blocking the HER2 receptor. Doctors often prescribe it in combination with trastuzumab and chemotherapy.
T-DM1 (Kadcyla) is also an option when treatment has already involved trastuzumab and chemotherapy.
When multiple therapeutic options have not worked, oncologists can weigh up other targeted options specific to a person’s condition.
Other HER2-targeted therapies include lapatinib (Tykerb) and neratinib (Nerlynx).
For people with cancer that is negative for the HER2 receptor and positive for the estrogen or progesterone receptors, an additional option includes palbociclib (Ibrance). This inhibits the enzymes cyclin-dependent kinase (CDK) 4 and 6. Letrozole or fulvestrant are other alternatives, which are anti-hormone receptor therapies for postmenopausal hormone blockade.
Other CDK4/6 inhibitors include ribociclib (Kisqali) and abemaciclib (Verzenio).
Targeted treatments can cause side effects. Medical teams will carefully monitor for these effects during and after the treatment.
Trastuzumab, for example, can affect heart function in some people. It causes a left ventricular ejection fraction (LVEF) decline in
Many medical centers have cardio-oncology programs in which oncologists and cardiologists work together to optimize heart health during cancer treatment.
Other side effects associated with some targeted treatments
Members of the medical team will describe the side effects of each treatment and work together to help manage them.
Sometimes, if side effects are intolerable or too harmful, oncologists recommend a change in therapy.
When MBC progresses during treatment, there may be other therapeutic options specific to the tumor profile.
Advances in treatment for MBC continue to evolve, and other options often exist. Before implementing any, medical teams must consider the individual tumor factors and the person’s overall condition.
Joint decision making is an important part of MBC management. It is important that oncologists discuss the various considerations with the person and ask for their thoughts before implementing a treatment plan.
For anyone with a cancer diagnosis, it is easy to feel a loss of control. It is important to remember that the members of the medical team are partners in a person’s care and that support networks are available.
In addition to providing tailored treatment options, there is also a focus on improving the quality of life and reducing the side effects of the treatment that negatively affect it.
Stress reduction techniques, such as meditation and yoga, can positively affect the quality of life. The effect of yoga on people with breast cancer requires more research, but some evidence suggests that it is associated with decreased fatigue, improvements in sleep, and a better quality of life overall.
Studies have also shown that exercise can reduce pain and fatigue in people with MBC.
Maintaining a moderate weight for overall health and well-being is also important for anyone with cancer, regardless of its stage.
Researchers do not yet fully understand the effect of obesity on breast cancer progression. However, there is
In general, people with MBC should avoid alcohol and follow a diet rich in fruits and vegetables.
Researchers are continuously engaging in and evaluating MBC studies. Clinical trials can help oncologists identify new treatment options — ideally, those that offer improved outcomes with few side effects.
People can find clinical trials on various websites, including those of the
Medical teams will assess whether a person is a suitable candidate.
There is no one-size-fits-all outlook for people with MBC. When determining an outlook, a doctor must consider the individual’s context and tumor profile.
Dr. Michelle Azu is a breast surgical oncologist who completed her breast surgery fellowship training in 2009 at Memorial Sloan Kettering in New York City. Currently, Dr. Azu is the director of breast surgery at a regional network hospital for a healthcare system in New York City. She is also an assistant professor of surgery for an academic institution in New York City.
Dr. Azu always looks forward to new opportunities to share advances in breast cancer research. She has received numerous honors throughout her career and makes every effort to provide outstanding, evidence-based, compassionate care tailored to her patients.