Severe psoriasis causes severe plaques, inflammation, itching, and shedding. It could be painful and impact a person’s quality of life. Treatments include medications, ointments, and light therapy.

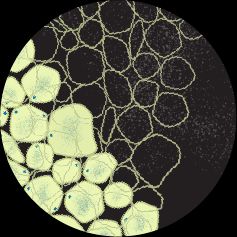
Psoriasis is an autoimmune disease. It causes new skin cells to grow too quickly and build up in thick, scaly, and colored plaques.
Many treatments for psoriasis are available. But doctors will often consider a different treatment approach for people with severe psoriasis compared to those with a mild or moderate form of the condition.
In this article, we discuss severe psoriasis and treatment options that may help a person manage their symptoms.
Experts classify psoriasis as mild, moderate, or severe.
A person with severe psoriasis may experience severe inflammation, itching, and skin shedding that could negatively impact their quality of life.
In the same 2021 study referenced above, researchers noted that approximately
Doctors may consider a range of factors when determining the severity of a person’s symptoms, including:
- symptom intensity
- location of symptoms
- the impact on a person’s daily life
They may use different
- Body surface area (BSA): This assessment method looks at how much of a person’s
BSA psoriasis affects. For reference, a person’s hand is considered 1% of their total BSA. - Psoriasis area and severity index (PASI): This method measures the severity of a person’s psoriatic symptoms and their response to treatment. A
PASI score may then indicate a person’s severity of psoriasis. - Dermatology life quality index (DLQI): This assesses the
impact of symptoms on a person’s quality of life, as people with psoriasis often experience anxiety, depression, and social isolation.
| Severity of psoriasis | BSA affected | PASI score |
|---|---|---|
| mild | less than 3% | 0–4 |
| moderate | 3–10% | 5–9 |
| severe | more than 10% | 10+ |
Psoriasis is associated with inflammation in the skin. Typically, the more inflammation that is present in the skin, the more noticeable psoriasis lesions or plaques will appear on the skin.
This is important to keep in mind, as some assessment methods have limitations.
For example, the PASI measures the redness of lesions, but not all skin affected by psoriasis becomes red. Skin lesions on people with dark skin tones may become darker or take on a purplish hue, while people with brown skin may develop coral-colored plaques of skin.
Therefore, determining the presence of inflammation may be more helpful in identifying psoriasis severity.
Psoriasis treatment largely depends on the severity and location of symptoms.
Mild psoriasis may respond well to topical creams, lifestyle changes, and natural remedies.
However, severe symptoms often do not respond to these treatments. A doctor will likely prescribe biologic or systemic medication or a combination of treatment options to help manage symptoms and prevent flares.
In some cases, a person with severe psoriasis may also need to spend time in the hospital.
Biologic drugs are a relatively new type of drug that targets specific parts of the immune system to block inflammation and prevent the overproduction of skin cells. Examples include:
- adalimumab (Humira)
- certolizumab (Cimzia)
- ustekinumab (Stelara)
- etanercept (Enbrel)
- secukinumab (Cosentyx)
These drugs may be administered intravenously by a doctor or as a self-injection.
A doctor may also prescribe biologics if a person’s symptoms are mild but affect their face, hands, or genitals.
Three types of Janus kinase (JAK) inhibitors have been approved to help treat psoriasis in the United States and Europe. These drugs help reduce inflammation and psoriasis symptoms by
These drugs include:
- tofacitinib (Xeljanz)
- baricitinib (Olumiant)
- ruxolitinib (Jakafi)
Other systemic drugs may be cheaper than biologics and available in oral form. These may include:
- methotrexate
- deucravacitinib (Sotyktu)
- cyclosporine (Neoral)
- acitretin (Soriatane)
- apremilast (Otezla)
Systemic drugs affect the whole body but work in different ways. For example, methotrexate, cyclosporine, and apremilast suppress the immune system to reduce inflammation.
Acitretin, a retinoid, also reduces inflammation and affects skin cell production. However, it does not suppress the immune system. People who are pregnant should not handle acitretin or breathe in dust particles from it.
Biologic and other systemic drugs may have side effects. These drugs affect how the immune system works, and they can increase the risk of infections. For this reason, they may not be suitable for everyone.
A doctor may recommend a topical treatment alongside a systemic drug to help treat severe psoriasis. Topical therapies are the
These may include:
- corticosteroids
- tacrolimus and pimecrolimus, which are calcineurin inhibitors
- vitamin D analogs
- retinoids, such as tazarotene (Tazorac)
- moisturizers and emollients
- tapinarof (Vtama)
- roflumilast (Zoryve)
- salicylic acid
- anthralin
- coal tar
Topical treatments may have adverse effects, such as burning, irritation, or increased susceptibility to UV light. People should speak with a medical professional before using any product.
Light therapy is a first-line treatment for guttate psoriasis. It may also be an option for people whose symptoms no longer respond to topical treatments, or for people who do not yet feel ready for systemic or biologic treatments.
The most common form of light therapy is controlled exposure to ultraviolet (UV) rays. This therapy is administered in a phototherapy center, but some people may be able to have treatment at home.
The drug psoralen may also help sensitize the skin to UVA light. The combined therapy of taking psoralen and being exposed to UV light is known as PUVA.
That said, ongoing research suggests that a person who receives more than
Some natural, alternative, or complementary therapies used alongside medical treatment may help with severe symptoms of psoriasis.
Home remedies may include:
- traditional Chinese medicine treatments
- herbal remedies, such as aloe vera and
St. John’s wort - dietary supplements, such as fish oil, vitamin D, turmeric, and zinc
- a gluten-free diet for people with a diagnosis of celiac disease
- mind and body wellness strategies, such as hypnosis and meditation
- stress management strategies, including cognitive behavioral therapy and guided imagery
There is not enough scientific evidence to support the use of these remedies. They may not be safe and effective for everyone. It is important that people talk with a doctor before starting any new treatment approach.
A doctor may also make recommendations regarding lifestyle measures, including:
- dietary changes
- getting regular physical activity like exercise
- quitting smoking if a person smokes
- limiting alcohol consumption if a person drinks alcohol
Smoking and drinking alcohol may trigger psoriasis flares and increase the risk of comorbidities. Experts strongly recommend people with psoriasis quit or avoid smoking and limit or avoid alcohol consumption.
Approximately 30–33% of people with psoriasis may develop psoriatic arthritis (PsA) around 10 years after their psoriasis symptoms first appear.
People with psoriasis may also have a higher risk of developing other conditions, such as:
- depression
- heart disease
- metabolic syndrome
some cancers , such as lung, lymphoma, bladder, and non-melanoma skin cancer
How serious is severe psoriasis?
Severe psoriasis can be very painful, and it may affect a person’s quality of life.
Some types of psoriasis may need urgent medical attention.
Erythrodermic, which is an uncommon type of psoriasis, may cause a painful rash that could cover large parts of the body and lead to life threatening complications.
Pustular psoriasis is also a rare and severe form of psoriasis that often requires inpatient hospitalization.
Severe psoriasis may cause pain and discomfort and may seriously affect a person’s quality of life.
Although there is currently no cure for psoriasis, various treatment options may help people with long-term management.
A doctor can help an individual develop a suitable treatment plan, which may need adjusting over time.