Erythrodermic psoriasis is an uncommon, aggressive, inflammatory form of psoriasis that typically requires immediate medical treatment. Symptoms include a peeling rash across the entire surface of the body.
Erythrodermic psoriasis is one of the most severe types of psoriasis and can be life threatening. The condition most often affects people who already have unstable plaque psoriasis. The rash that occurs with erythrodermic psoriasis can itch or burn intensely and spread quickly.
Rarely, it can also occur at the onset of an episode of plaque psoriasis or alongside another rare type of psoriasis called von Zumbusch pustular psoriasis.
The signs and symptoms of erythrodermic psoriasis can be intense.
Symptoms
Symptoms of erythrodermic psoriasis include:
- severe skin redness over a large part of the body
- skin shedding that occurs in large sheets rather than smaller flakes or scales
- pustules or blisters
- burnt-looking skin
- severe itching
- intense pain
- increased heart rate
- fluctuations in body temperature
These symptoms will affect most people during an erythrodermic psoriasis flare.
Erythrodermic psoriasis can alter the chemistry of the body. For this reason, people may also experience other symptoms.
These include:
Scientists are not sure exactly what causes psoriasis itself, but it appears to be due to an overactive immune system.
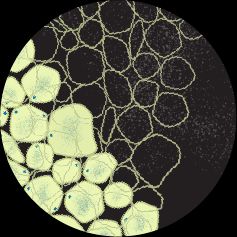
When a person has psoriasis, the body produces an excessive number of T cells, which are a kind of white blood cell that usually defends against bacteria and viruses.
In psoriasis, these T cells are erroneously activated and attack healthy skin cells. This causes an overproduction of skin cells and other symptoms.
The symptoms of psoriasis mostly appear on the skin, but the condition can also affect the nails, joints, and other parts of the body.
However, it remains unclear why erythrodermic psoriasis develops, though there are some known triggers. These include:
- stopping the use of medications for plaque psoriasis such as corticosteroids or immunosuppressants
- allergic reaction to a medication for psoriasis
- infection
- severe sunburn
- drinking alcohol
- stress
Erythrodermic psoriasis can be difficult to treat, especially if complications develop.
The first-line treatment is usually fast-acting immunosuppressants.
In some cases, the treatment may include topical steroid creams and moisturizers, biologics, as well as oral steroids. That said, doctors tend to avoid steroids because of the chance of a rebound after stopping the medication.
They may also choose to deliver the drug through an injection or an infusion.
A person’s emergency treatment options will depend on the severity of their symptoms and the presence of any other health conditions.
Emergency treatment consists of intravenous (IV) fluid and electrolyte replacement to treat or prevent dehydration.
Drug treatment
The immunosuppressants cyclosporine (Neoral, Gengraf, Sandimmune) and Remicade (infliximab) are standard
In less severe cases, a doctor may prescribe methotrexate (Otrexup) or acitretin (Soriatane) instead.
Once a person’s condition is stable, the doctor may recommend changing to another drug, possibly Enbrel (etanercept), or using combination therapy.
Biologics
Biologic drugs, such as etanercept or Humira (adalimumab), which are tumor necrosis factor (TNF)-alpha inhibitors and some interleukin (IL) inhibitors, can also be an effective treatment for moderate to severe erythrodermic psoriasis.
Newer biologics target different genes.
Other treatment
A doctor may also prescribe antibiotics to prevent or treat other infections if necessary.
The person may need to spend time in the hospital. However, outpatient treatment may be possible if their condition is stable and they are not losing fluids. The person may need bed rest.
People with HIV
Psoriasis in people living with HIV may be more challenging to treat, including erythrodermic psoriasis.
For a person with HIV and erythrodermic psoriasis,
Other treatments may not effectively treat erythrodermic psoriasis in people with HIV.
The skin acts as the body’s barrier layer, which is crucial to overall health.
Severe skin damage resulting from erythrodermic psoriasis disrupts the environment of the entire body.
The body
- severe illness from loss of protein or fluid
- excessive swelling from fluid retention
- severe infections, including pneumonia and sepsis
- high output heart failure
Complications due to bacterial infection can become life threatening.
Doctors can usually identify erythrodermic psoriasis with a physical examination. Most laboratory tests are not specific enough to confirm a diagnosis.
A person who has severe redness and peeling covering
The doctor will also check for signs of infection, as extensive damage to the skin will leave the body vulnerable.
It is crucial that anyone who notices any symptoms of erythrodermic psoriasis gets immediate medical attention because severe, life threatening complications may occur.
In some cases, doctors may admit the individual to the hospital.
People with psoriasis should follow their prescribed psoriasis routine and avoid specific triggers to help prevent an episode of erythrodermic psoriasis.
Triggers may
- stress
- cold weather
- wind
- excessive alcohol consumption
- smoking
However, sometimes the onset of erythrodermic psoriasis is sudden, making it hard to avoid the potential triggers.
Is erythrodermic psoriasis life-threatening?
Erythrodermic psoriasis can affect
What is the mortality rate for erythrodermic psoriasis?
While many cases are treated successfully, research data suggests that erythrodermic psoriasis can lead to death in as many as
What is the drug of choice for erythrodermic psoriasis?
Typically doctors prescribe the immunosuppressants cyclosporine and infliximab as first-line treatments for severe or unstable erythrodermic psoriasis. In less severe cases, they may prescribe other medications like methotrexate or acitretin.